Sustaining a NWD System requires a comprehensive strategy to blend various funding streams. Statewide governance including the ability to leverage existing funding remains a key component of successful development and implementation of a mature NWD. NWD Systems use a variety of funding streams with the largest percentage (over 50 percent) coming from state and local funds and only one percent from a federal NWD grant (NWD Business Case Grantee Reporting, 2019). ACL’s Strategic Framework for Action encourages this blending and braiding of funding sources. Funding sources NWD Systems use for development and operations include federal dollars such as the Older Americans Act (i.e. Information and Referral), the Rehabilitation Act (i.e. vocational rehab), the Omnibus Budget Reconciliation Act (i.e. State Health Insurance Counseling Program grants), and the Development Disabilities Act (i.e. University Centers for Excellence in Developmental Disabilities Education, Research, and Service). Additionally, NWD Systems have leveraged the following types of funding:
Medicaid (Medicaid Managed Care, Medicaid Administrative Funding, fee for service)
State General Funds
Veterans Health Administration programs
Medicare (Medicare Advantage, Medicare Special Needs Plans)
Hospital Systems
Health Plans
Public/Private Partnerships
Leveraging federal dollars requires a strong NWD System governing structure to coordinate and identify efficient and effective ways to use federal funds. Medicaid Administrative Claiming in particular requires an established partnership with the State Medicaid Agency. More resources on how to forge this relationship can be found below. Obtaining new and non-traditional funding such as health plans and health systems requires innovation and development of new partnerships which often require a greater degree of business acumen. In addition, ACL developed a business case toolkit available at https://www.ta-community.com/category/nwd-system-business-case-toolkit.
Medicaid Administrative Claiming is one avenue for sustaining and supporting a NWD System Medicaid claiming, also known as Federal Financial Participation (FFP), represents a way in which Federal funds are used to reimburse agencies doing work that supports Medicaid programs.
The role that NWD System’s play in assisting individuals with understanding and navigating complicated long-term services and supports includes many administrative functions that are eligible for Medicaid claiming.
Federal matching funds under Medicaid are available for costs incurred by the state for administrative activities that directly support efforts to identify and enroll individuals into Medicaid and that directly support the provision of services covered under the Medicaid state plan, when those activities are performed either directly by the state Medicaid agency or through contract or interagency agreement by another entity. The state Medicaid agency will advise the state’s NWD System Lead Agency on the essential infrastructure needed to claim Medicaid administrative funds. Often times, infrastructure is modeled after programs that have Medicaid claiming in place. Below are some key questions for NWD Systems to consider as Medicaid administrative funding is explored:
The NWD System activities that may be funded under Medicaid include:
Outreach
Person-Centered Counseling
Facilitating Medicaid Eligibility
Training
Programing Planning
Quality Improvement
The Centers for Medicare & Medicaid Services (CMS), in conjunction with ACL, made available on the CMS website a guidance document. This guidance outlines the basics of how states can draw down Medicaid administrative FFP for NWD Systems.
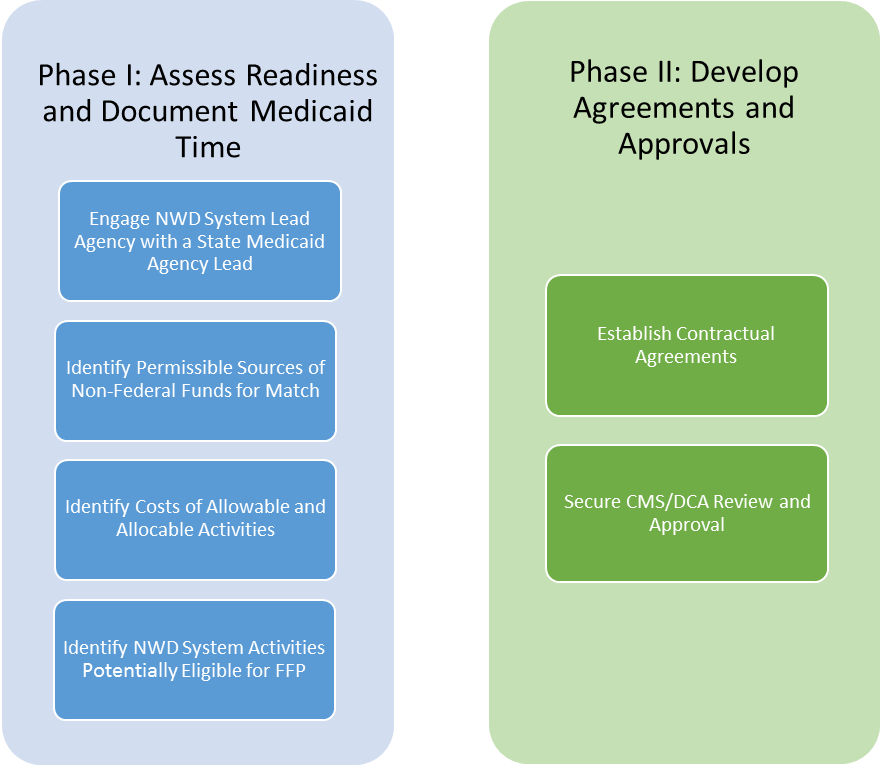
For further guidance, ACL has outlined the following steps across two phases of NWD System Medicaid administrative claiming development:
Want to learn more about other claiming
opportunities?
Check out this information on NWD
IT and PASRR Medicaid Claiming